置換人工關節手術
|
人工關節的風險? |
 |
很多病人選擇做人工關節手術之前,有沒有認真了解和衡量過做此手術的必要呢?
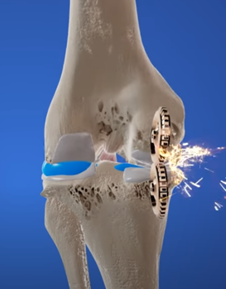
人工關節的平均壽命只有5-10年,全要原因是人工關節永遠無法與自身骨質融合,隨著時間與活動的增加,假體會容易出現鬆脫或滑落等問題。所以醫生通常建議病人65歲後才做手術,若過於年輕做手術,5-10年後可能需要重做手術,而且效果一定不會理想。
根據統計顯示: 5個人當中,就有1個人不滿意全膝關節置換手術。雖然現代人工關節手術技術和材料已經提高了安全性,但手術本質問題仍然存在(人工關節無法與自身骨質融合) |
更換人工關節的4個常見錯誤觀念
|
|
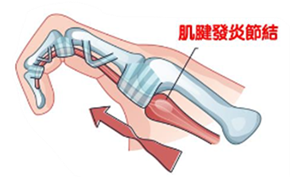
人工關節手術存在一定的風險 手術風險:
術後恢復風險:
由此可見,手術眾多的風險,併發症和後遺症,是O型膝痛的最後方法。 |
但為什麼醫生還推介病人做?事實上,醫院/器械公司/保險公司等利益者,為求牟利,暗地裏在各方面鼓吹和合謀,讓手術成為治療主流,但他們隱瞞了手術的本質問題,手術並非萬能,不但會破壞患處週邊的組織,而且長遠沒有解決原本疼痛問題。 |
病人應如何解決O型膝痛?面對手術眾多的風險,併發症和後遺症,病人應該及時進行正確的保守治療(矯形器K39d)和矯正,不但無風險,無負作用,更可有效打開膝內側空隙,解決O型膝痛。 從而避免人工關節置換手術,減少手術帶來的風險,併發症和後遺症。 |
|
(若能跟隨以下保守療法指南, 便可避免做手術) 保守療法指南 |
| 選擇[精準有效的保守療法] | 避免[不良姿勢],[不良動作] | 配合恰當的[混合治療] |
| 堅持與耐性 | 並廣傳[病從淺中醫]的理念 | 應諮詢多位專家的意見 |
|
人工關節置換手術過程覆雜,且手術最終一定鬆脫 |
|
手術是一種不可逆轉的程序, 而且過程需破壞大量原有組織,更需承受風險, 並發症, 後遺症, 一齊黎睇下依個手術嘅覆雜程序! 以下是手術的步驟: |
|
瀏覽為
排序由
顯示
每頁
K39d-免負重膝矯形器(O型腳)
膝骨性關節炎
適用症狀:
✔️錯位 ✔️畸形 ✔️負重疼痛 ✔️半月板撕裂 ✔️ 單邊骨性關節炎<歡迎來電預約免費佩戴,體驗減痛效果>
需要預約 請點擊下列連結
HK$5,800.00
K39f-免負重膝矯形器
膝骨性關節炎
適用症狀:
- 單邊骨性關節炎- 力線不正(X型腳)
- 膝關節不穩
- 任何單側傷患或疼痛,要避免負重,即可使用
- 半月板撕裂、修補及移植 <歡迎來電預約免費佩戴,體驗減痛效果>
HK$5,800.00
HK$5,220.00